developed by: University of Iowa Health Care researchers
 Excerpted from Currents: Fall 2000-Winter 2001, Volume 2, Number 1
Excerpted from Currents: Fall 2000-Winter 2001, Volume 2, Number 1
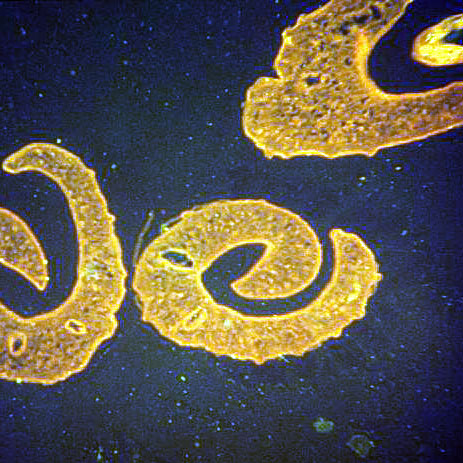
Will Helminths Become the Future Treatment for Inflammatory Bowel Disease?
by Joel Weinstock, M.D., and William R. Summers, M.D.
The Hygiene Hypothesis:
* Organisms that live in human intestines are important for toning and shaping both the local immune system and the systemic immune responses
* The progressive hygienic styles characteristic of industrialized societies have removed people from their natural surroundings, which drove adaptation of the human immune system, and now provide an intestinal environment far different from that of our ancestors
* This difference is leading to the emergence of various autoimmune and other types of immunological diseases
* Loss of helminthic colonization and the unique impact of these parasites on our immune response are major factors contributing to the development of autoimmune diseases
History: Epidemiologic studies show that inflammatory bowel disease1 (IBD) is most common in Western industrialized countries that are characterized by affluent societies living in sanitized environments. Alternatively, IBD is rare in developing countries with less clean environments and more crowded living conditions. The explanation for this difference has always been speculative, but it is a well-established epidemiological fact that the prevalence of IBD is inversely proportional to the prevalence of helminthic parasites in the same population.
IBD likely results from dysregulated immune responses to intestinal contents. As the immune system reacts to foreign proteins, inflammatory cells simultaneously secrete and respond to cytokines that regulate the reaction. Two counter-regulatory patterns of cytokine secretion can be identified in many immune responses. Polarized Th21 responses impede expression of Th2 cytokines, whereas polarized Th2 responses impede Th1 pattern of activity. The Th1 response is characterized by an increase in IL3-12 and IFN-gamma4. The Th2 response involves increased IL-4, IL-5, and IL-13. Crohn’s disease is an overly active and destructive Th1 inflammatory response, possibly induced by intestinal bacteria. The cytokine profile in active ulcerative colitis (UC) shows significant IFN-gamma release but is not as polarized as that seen in Crohn’s disease. The pro-inflammatory cytokines IL-1ß, IL-6, IL-8 and TNF-alpha 5 increase in both UC and Crohn’s disease.
Under experimental conditions, the immune response induced in the host by intestinal helminths is characterized by a Th2 pattern of cytokine release and a non-specifically down-regulated Th1 reactivity. Indeed, a number of helminths have been shown to induce Th2-type inflammation thus down-modulating the Th1 type of immune responses to unrelated bacterial or viral infections. Thus, people carrying helminths would be more apt to mount a subdued Th1 response when challenged with other antigens. This may prevent an overly exuberant Th1 inflammatory response at mucosal surfaces like that occurring in Crohn’s disease. Alternatively, genetically susceptible persons never exposed to helminths might lack a strong counter-active Th2 immune response and develop a poorly regulated and destructive intestinal Th1 response resulting in chronic colitis or ileitis.
New facts: Following the above logic, a group of University of Iowa Health Care researchers has proposed that the absence of exposure or underexposure to intestinal helminths is a major environmental factor predisposing to IBD. This hypothesis is grounded in epidemiological data showing that the incidence of Crohn’s disease in industrialized societies increased from the 1950s until the mid-1980s, particularly, in temperate regions. This increase was preceded by a sharp drop in the incidence of parasitic worm infection, which, prior to the 1930s, were harbored by nearly all children living in the southeastern regions of the U.S. In the 1940s, one in six Americans showed signs of previous Trichinella exposure on routine autopsy. This decreased to less than 5% by the 1960s, with only 0.5% showing signs of recent infection.
The hypothesis was first tested using murine models of Th1-driven intestinal inflammation. Schistosomiasis (pre-exposure to S. mansoni) prevented colitis development in mice rectally challenged with tri-nitrobenzene-sulfonic acid and ethanol. The pre-exposure diminished Th1 and augmented Th2 responsiveness thus protecting mice from developing colitis. In another model-mice with disrupted IL-10 genes that develop severe colitis due to excessive Th1 responses to colonic content-exposure to the intestinal helminth H. polygyrus significantly reduced intestinal inflammation. Intestinal inflammation was also significantly attenuated in IL-10 deficient mice by exposure to Trichuris muris.
It is important to note that other autoimmune, Th1-driven inflammatory diseases, such as multiple sclerosis (MS) and type 1 diabetes, share the epidemiologic characteristics of IBD. MS, for example, is rare in tropical countries and is more common in industrialized temperate regions. Concurrently, colonization with helminthic parasites has become less common in the latter while remaining unchanged in the former. MS results from an exuberant Th1 immune response probably directed against a peptide sequence shared by a virus/bacterium and cells that make myelin. Since initial exposure to viruses or bacteria usually occurs at mucosal surfaces, mucosal Th2 conditioning may prevent dysregulated Th1 reactivity to such shared peptide sequences.
Clinical relevance: The possibility that intestinal helminths might protect their host from developing or maintaining IBD led the UI Health Care group to consider the use of one such agent in the treatment of active IBD. The ideal agent would colonize the intestine without invading the host. In addition, the source of the helminth needed to be pathogen-free to minimize the risk of co-transmitting other diseases that represent public health hazard, such as HIV or hepatitis B, C, or E. The porcine whipworm, Trichuris suis, meets these requirements.
T. suis is not a human parasite, but its ova are capable of colonizing a human host for several weeks and are eliminated thereafter without any specific therapy. Eggs that are shed in the stool are not capable of colonizing because they are not yet embryonated. This helminth cannot be cultured or raised in vitro but can be harvested from colonized pathogen-free pigs.
Eight patients who had steroid-dependent or resistant IBD involving the colon and/or small bowel (five had Crohn’s disease and three had UC) were chosen for a pilot study using T. suis eggs. Each of the subjects was given either a single dose of 2,500 eggs in 30 ml of Gatorade or one dose weekly for three weeks.
Patient evaluation included stool frequency, Crohn’s disease activity index (CDAI), complete blood count, hepatic enzymes and bilirubin, erythrocyte sedimentation, C-reactive protein, urinalysis, stool for culture, ova and parasite examination, and IBD quality of life questionnaire (IBDQ). Although in IBD no single laboratory study adequately describes the degree of active inflammation, the effect of treatment was clearly reflected in positive changes to the evaluation criteria matching a subjective perception of improvement.
The lowest CDAI values, for example, occurred from four to 12 weeks (mean seven weeks) after the study started, and the mean lowest value was 55% of the initial value (p=0.03). Four of the five patients with Crohn’s disease achieved remission (CDAI lower than 150), and the fifth had a significant 151 point reduction in CDAI.
The IBDQ rose in all patients from an initial mean value of 124 to the highest mean value of 186 (p=0.00005). An IBDQ of 170 or higher is often considered remission, and following this criterion, seven of eight patients achieved remission that lasted up to five months.
While there was considerable variability, the mean number of stools per week decreased in all subjects from 59 to 33, or about 50% of the initial value (p=0.03).
Finally, all patients assessed their subjective feeling of improvement on a nine point Likert scale (1 = severe exacerbation, 9 = complete remission): the mean response value was 7.5. The mean duration of the response was five weeks.
No significant complications or adverse events occurred in any of the patients. No patient expressed any concern during or after the study about the therapy, and all were willing to undergo additional treatments.
All patients relapsed after a single dose. The cause of relapses was unknown, but it seemed plausible that they occurred because of subtle changes in the environment that affected the Th1-Th2 balance. Since T. suis only colonizes humans briefly, it is assumed that the duration of Th2 response to this organism was not sufficient to permanently shift the balance away from an abnormal Th1 response.
Thus, the investigators were given permission to administer a maintenance dose of the agent every three weeks to patients with refractory IBD. Two patients with Crohn’s disease and two with UC were entered into the second phase of the open-label study. All four patients went into sustained remissions. Two of them have received this treatment for more than a year now. A double-blind study is now under way to further test the efficacy of this therapy.
Two epidemiologic findings are relevant to the hygiene hypothesis framing this situation: a) people in areas endemic for intestinal helminths are protected from IBD; and b) at the same time, the majority of them do not develop disease directly attributable to intestinal helminths. Their immune system seems adapted to helminthic colonization and, therefore, these parasites may play a vital role in preventing immune dysregulation in genetically susceptible individuals. By ridding ourselves of relatively harmless organisms with a relevant immunoregulatory role, we may have inadvertently produced an immunoregulatory imbalance and thus have become prey to autoimmune diseases like IBD.
Helminths that colonize the human gastrointestinal system:
* Nematodes (round worms):
o Enterobius vermicularis (pin worm), Trichuris trichiura (whipworm)
o Ancylostoma duodenale and Necator americanus (hookworms), Ascaris
* Platyhelminths (flat worms):
o Trematodes (flukes): Fasciolopsis spiralis, Echinostoma spiralis, Heterophyes spiralis, Clonorchis sinensis, Opisthorchis viverrini, Opisthorchis felineus, Fasciola hepatica, Schistosoma mansoni, and Schistosoma japonicum
o Cestodes (tape worms): Diphyllobothrium spiralis, Taenia saginata, Tenia solium
source: Currents: Fall 2000-Winter 2001, Volume 2, Number 1





I’d love to hear from anyone who has done this therapy! Please contact me through my Planet Thrive “earthwalker” profile.
Please let me know if anyone with MS has used this therapy and had success. I have just had my 2nd episode and am 56 years old.